The Comprehensive Guide to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)
Introduction
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) is a critical tool in the field of mental health. It provides standardized criteria for diagnosing mental disorders, ensuring consistency and reliability in clinical practice and research. At ivyleagueassignmenthelp.com we help and guide students to explores the history, structure, and significance of the DSM-5, detailing its impact on modern psychiatry.
History of the DSM
The DSM has evolved significantly since its inception. The first edition, DSM-I, was published in 1952 by the American Psychiatric Association (APA). Over the decades, the manual has undergone several revisions to reflect advances in psychiatric research and changes in societal attitudes towards mental health. Key milestones include:
- DSM-I (1952): Introduced to provide a standardized language for psychiatric diagnosis.
- DSM-II (1968): Expanded to include more disorders and reflected the influence of psychoanalytic theory.
- DSM-III (1980): Marked a shift towards a more empirical and research-based approach, introducing explicit diagnostic criteria.
- DSM-III-R (1987): Revised to correct inconsistencies and improve reliability.
- DSM-IV (1994): Incorporated findings from extensive field trials and included a multi-axial system for assessment.
- DSM-IV-TR (2000): Updated text and criteria based on new research.
- DSM-5 (2013): The latest edition, featuring significant structural and content changes, including the removal of the multi-axial system.
Purpose and Importance of the DSM
The DSM serves several crucial purposes:
- Standardization: Provides a common language for diagnosing mental disorders, facilitating communication among clinicians, researchers, and policymakers.
- Clinical Practice: Guides clinicians in diagnosing and treating patients, ensuring that diagnoses are based on reliable and validated criteria.
- Research: Serves as a foundation for research on mental disorders, allowing for consistency in study design and interpretation.
- Insurance and Policy: Influences insurance coverage and health policy decisions by providing clear definitions of mental disorders.
Structure of the DSM-5
The DSM-5 is organized into three main sections:
- Introduction and Use: Provides an overview of the manual and instructions for its use.
- Diagnostic Criteria and Codes: Detailed descriptions of mental disorders, including criteria for diagnosis, associated features, and differential diagnoses.
- Emerging Measures and Models: Includes assessment tools and models for further research and clinical practice.
The manual is divided into chapters based on broad diagnostic categories, such as mood disorders and anxiety disorders, each containing specific diagnoses with criteria and codes.
Major Diagnostic Categories in the DSM-5
The DSM-5 categorizes mental disorders into several major groups. Here are some key categories:
- Mood Disorders: Including major depressive disorder and bipolar disorder.
- Anxiety Disorders: Including generalized anxiety disorder, panic disorder, and phobias.
- Psychotic Disorders: Including schizophrenia and schizoaffective disorder.
- Neurodevelopmental Disorders: Including autism spectrum disorder and ADHD.
- Personality Disorders: Including borderline personality disorder and antisocial personality disorder.
- Substance-Related and Addictive Disorders: Including alcohol use disorder and gambling disorder.
- Trauma- and Stressor-Related Disorders: Including PTSD and acute stress disorder.
- Eating Disorders: Including anorexia nervosa and bulimia nervosa.
- Obsessive-Compulsive and Related Disorders: Including OCD and hoarding disorder.
- Sleep-Wake Disorders: Including insomnia and narcolepsy.
- Sexual Dysfunctions and Gender Dysphoria: Including erectile disorder and gender dysphoria.
- Neurocognitive Disorders: Including Alzheimer’s disease and delirium.
Mood Disorders in the DSM-5
Mood disorders are characterized by disturbances in mood that affect functioning. Major depressive disorder and bipolar disorder are two primary examples. The DSM-5 provides specific criteria for these disorders, including symptoms, duration, and impact on daily life.
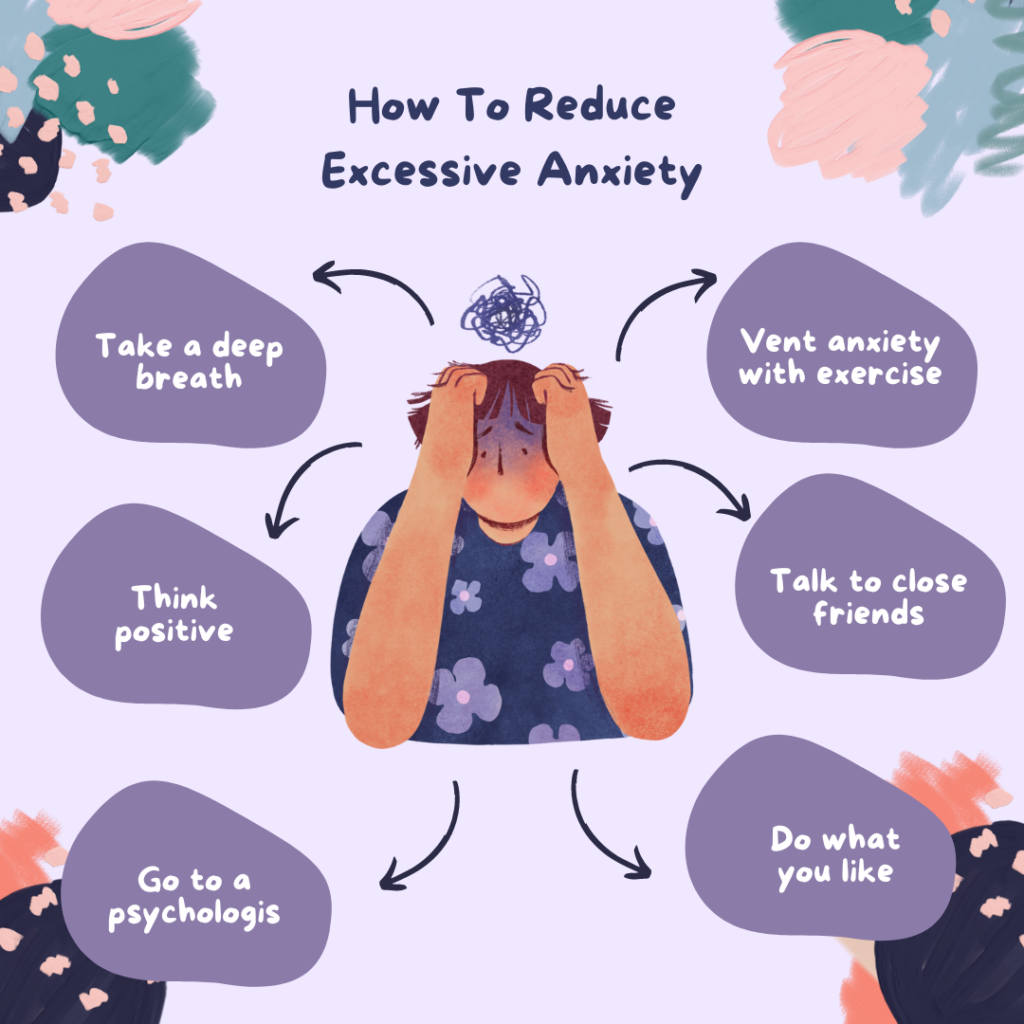
Anxiety Disorders in the DSM-5
Anxiety disorders involve excessive fear or anxiety. Generalized anxiety disorder, panic disorder, and specific phobias are among the most common. The DSM-5 outlines criteria for diagnosis, focusing on the intensity and duration of anxiety symptoms.
Psychotic Disorders in the DSM-5
Psychotic disorders, such as schizophrenia, involve distorted thinking and perceptions. The DSM-5 criteria for these disorders include symptoms like hallucinations, delusions, and disorganized speech.
Neurodevelopmental Disorders
Neurodevelopmental disorders typically manifest early in development and include conditions like autism spectrum disorder and ADHD. The DSM-5 provides detailed criteria for diagnosing these disorders, emphasizing developmental history and symptomatology.
Personality Disorders
Personality disorders are characterized by enduring patterns of behavior and inner experience that deviate from cultural expectations. The DSM-5 lists ten personality disorders, including borderline and antisocial personality disorders, with criteria focusing on pervasive and inflexible traits.
Substance-Related and Addictive Disorders
These disorders involve the problematic use of substances like alcohol and drugs, as well as behaviors like gambling. The DSM-5 criteria include patterns of use, impairment, and distress.
Trauma- and Stressor-Related Disorders
Disorders like PTSD result from exposure to traumatic or stressful events. The DSM-5 criteria for these disorders include the nature of the trauma, symptom clusters, and duration.
Eating Disorders in the DSM-5
Eating disorders involve severe disturbances in eating behavior. Anorexia nervosa and bulimia nervosa are two primary examples, with the DSM-5 criteria focusing on eating patterns, body image, and health impact.
Obsessive-Compulsive and Related Disorders
These disorders are characterized by obsessive thoughts and compulsive behaviors. The DSM-5 includes OCD and related disorders like hoarding disorder, with criteria emphasizing the nature and impact of obsessions and compulsions.
Sleep-Wake Disorders
Sleep-wake disorders involve disruptions in sleep patterns. The DSM-5 includes disorders like insomnia and narcolepsy, with criteria focusing on sleep quality, duration, and impact on daily functioning.
Sexual Dysfunctions and Gender Dysphoria
These disorders involve issues related to sexual functioning and gender identity. The DSM-5 includes criteria for conditions like erectile disorder and gender dysphoria, addressing symptoms and distress.
Neurocognitive Disorders
Neurocognitive disorders involve cognitive decline from a previous level of functioning. Alzheimer’s disease and delirium are key examples, with DSM-5 criteria focusing on cognitive impairments and their impact on daily life.
Criticisms and Controversies of the DSM-5
The DSM-5 has faced criticisms regarding its reliability, validity, and potential for overdiagnosis. Some argue that it medicalizes normal variations in behavior, while others criticize its categorical approach to diagnosing mental disorders.
Cultural Considerations in the DSM-5
The DSM-5 acknowledges the importance of cultural context in diagnosing mental disorders. It includes a cultural formulation interview to help clinicians consider cultural factors in diagnosis and treatment.
Use of the DSM-5 in Clinical Practice
Clinicians use the DSM-5 to diagnose mental disorders, inform treatment planning, and communicate with other healthcare professionals. The manual’s standardized criteria ensure consistent and reliable diagnoses.
Future Directions for the DSM
Future updates to the DSM may include revisions based on new research, improved diagnostic criteria, and integration with digital health technologies. Ongoing research aims to refine our understanding of mental disorders and improve diagnostic accuracy.
Case Studies Using the DSM-5
Case studies illustrate the practical application of the DSM-5 in clinical settings. These examples highlight the diagnostic process, use of criteria, and development of treatment plans based on DSM-5 guidelines.
Comparison with Other Diagnostic Manuals
The DSM-5 is often compared with the International Classification of Diseases (ICD). While both provide criteria for diagnosing mental disorders, they have differences in structure, classification, and global usage.
Training and Education on the DSM-5
Training on the DSM-5 is crucial for clinicians, students, and researchers. Resources include workshops, courses, and manuals to ensure accurate and effective use of the DSM-5 in practice.
FAQs
What is the DSM-5?
The DSM-5 is the latest edition of the Diagnostic and Statistical Manual of Mental Disorders, providing standardized criteria for diagnosing mental disorders.
How is the DSM-5 used in clinical practice?
Clinicians use the DSM-5 to diagnose mental disorders, inform treatment planning, and ensure consistent and reliable diagnoses.
What are some major changes in the DSM-5 compared to previous editions?
Major changes include the removal of the multi-axial system, new and revised diagnostic criteria, and the inclusion of emerging measures and models.
Why is the DSM-5 important in mental health research?
The DSM-5 provides standardized criteria that ensure consistency in research studies, enabling accurate data collection and comparison across studies.
What are some criticisms of the DSM-5?
Criticisms include concerns about reliability and validity, potential for overdiagnosis, and the medicalization of normal behavior variations.
How does the DSM-5 address cultural considerations?
The DSM-5 includes a cultural formulation interview to help clinicians consider cultural factors in diagnosis and treatment.
